
Contributions
Abstract: PB2106
Type: Publication Only
Background
Azacitidine (AZA) was the first drug demonstrating survival benefit over conventional care in patients with high risk MDS, including AML with 20-30 % blasts. It has been the standard of care in patients not eligible for allogeneic stem cell transplantation and is lately also used in elderly patients with AML. The medication is usually well tolerated. We will report two patients with cutaneous side effects of AZA, which turned into a life-threatening systemic affection in one of them.
Aims
By these cases, we want to demonstrate that AZA can cause life-threatening skin lesions. High-dose steroids can dramatically improve a nearly fatal clinical situation.
Methods
The two patients included in this report have both given written informed consents to this publication. We describe two patients who have been treated at a local and a university hospital.
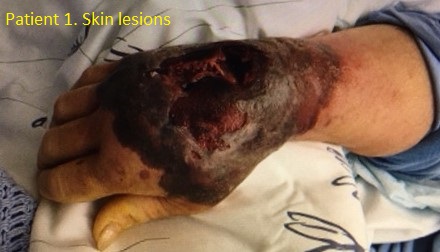
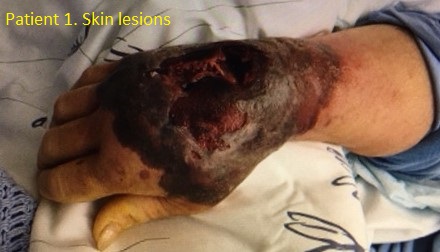
Patient 1 was a 79-year-old woman with MDS-EB-2 treated with AZA 100 mg/m2 subcutaneously (sc) days 1-5. She was admitted to hospital on day 5 because of dyspnea, coughing and high fever. Chest X-rays showed a consolidation. She was treated with broad-spectrum antibiotics. After 7 days she developed darkly red and swollen skin lesions on her right hand. This rapidly changed into necrotic tissues as demonstrated at the picture. In addition, 3 more necrotic skin lesions were observed, also affecting her other hand. Surgery was performed several times. She became critical ill and circulatory instable with low blood pressure. It was considered unlikely that she would survive. Since no bacteria were found and AZA can give necrotizing fasciitis, acute febrile dermatosis and lung infiltrations, we as a last try, started with high-dose steroids. Within a short time, her condition was dramatically improved.
Patient 2 was a 72-year-old man with relapse of AML. He was treated with AZA 100 mg/m2 sc day 1-5. Before cycle 4, he was admitted to hospital because of neutropenic fever and received empirically broad-spectrum antimicrobials. Feeling better after 4 days he started AZA cycle 4.The following day he rapidly developed darkly red and swollen skin lesions on both hands and forearms in addition to high fever. The similarity between his skin affection and the findings in patient 1, made us consider AZA-induced side effects likely. We chose to treat him with high-dose steroids. Already the next day his condition had improved.
Results
For patient 1 laboratory values revealed neutrophils 42.3x109/L. Microbiological samples from skin and blood were all negative. Biopsy of the skin lesions showed neutrophilic dermatosis as in Sweet syndrome.
For patient 2 a skin biopsy showed subacute inflammation with no signs of vasculitis or infection, but findings comparable with drug-induced changes.
Conclusion
AZA-induced Sweet syndrome appears to be the cause of the progressing, necrotic skin lesions with the fulminant systemic affection and circulatory collapse in patient 1. High-dose steroids dramatically improved her situation. A similar development may have been prevented by introducing steroids to patient 2.
Session topic: 10. Myelodysplastic syndromes – Clinical
Keyword(s): Azacitidine, Corticosteroids
Abstract: PB2106
Type: Publication Only
Background
Azacitidine (AZA) was the first drug demonstrating survival benefit over conventional care in patients with high risk MDS, including AML with 20-30 % blasts. It has been the standard of care in patients not eligible for allogeneic stem cell transplantation and is lately also used in elderly patients with AML. The medication is usually well tolerated. We will report two patients with cutaneous side effects of AZA, which turned into a life-threatening systemic affection in one of them.
Aims
By these cases, we want to demonstrate that AZA can cause life-threatening skin lesions. High-dose steroids can dramatically improve a nearly fatal clinical situation.
Methods
The two patients included in this report have both given written informed consents to this publication. We describe two patients who have been treated at a local and a university hospital.
Patient 1 was a 79-year-old woman with MDS-EB-2 treated with AZA 100 mg/m2 subcutaneously (sc) days 1-5. She was admitted to hospital on day 5 because of dyspnea, coughing and high fever. Chest X-rays showed a consolidation. She was treated with broad-spectrum antibiotics. After 7 days she developed darkly red and swollen skin lesions on her right hand. This rapidly changed into necrotic tissues as demonstrated at the picture. In addition, 3 more necrotic skin lesions were observed, also affecting her other hand. Surgery was performed several times. She became critical ill and circulatory instable with low blood pressure. It was considered unlikely that she would survive. Since no bacteria were found and AZA can give necrotizing fasciitis, acute febrile dermatosis and lung infiltrations, we as a last try, started with high-dose steroids. Within a short time, her condition was dramatically improved.
Patient 2 was a 72-year-old man with relapse of AML. He was treated with AZA 100 mg/m2 sc day 1-5. Before cycle 4, he was admitted to hospital because of neutropenic fever and received empirically broad-spectrum antimicrobials. Feeling better after 4 days he started AZA cycle 4.The following day he rapidly developed darkly red and swollen skin lesions on both hands and forearms in addition to high fever. The similarity between his skin affection and the findings in patient 1, made us consider AZA-induced side effects likely. We chose to treat him with high-dose steroids. Already the next day his condition had improved.
Results
For patient 1 laboratory values revealed neutrophils 42.3x109/L. Microbiological samples from skin and blood were all negative. Biopsy of the skin lesions showed neutrophilic dermatosis as in Sweet syndrome.
For patient 2 a skin biopsy showed subacute inflammation with no signs of vasculitis or infection, but findings comparable with drug-induced changes.
Conclusion
AZA-induced Sweet syndrome appears to be the cause of the progressing, necrotic skin lesions with the fulminant systemic affection and circulatory collapse in patient 1. High-dose steroids dramatically improved her situation. A similar development may have been prevented by introducing steroids to patient 2.
Session topic: 10. Myelodysplastic syndromes – Clinical
Keyword(s): Azacitidine, Corticosteroids


