
Contributions
Abstract: S1547
Type: Oral Presentation
Presentation during EHA23: On Sunday, June 17, 2018 from 08:30 - 08:45
Location: Room A1
Background
A significant percentage of patients with newly diagnosed diffuse large B-cell lymphoma (DLBCL) have concurrent follicular lymphoma (FL) or other low-grade B-cell lymphoma in tissue and/or bone marrow biopsies. Clinically these patients are usually treated in the same way as those with pure de novo DLBCL. However, it is unclear whether they also have identical outcomes compared with de novo DLBCL patients. As a result, whether to include these patients in clinical trials of DLBCL remains controversial.
Aims
To compare the clinical characteristics and outcomes of patients with de novo DLBCL, concurrent DLBCL and FL (DLBCL+FL), or concurrent DLBCL and other low-grade B-cell lymphoma (DLBCL+LG).
Methods
1448 patients with newly diagnosed DLBCL from March 2002 to April 2015 were included in this study. Patients were enrolled in the Molecular Epidemiology Resource (MER) of the University of Iowa/Mayo Clinic lymphoma Specialized Program of Research Excellence (SPORE), treated with standard immunochemotherapy and followed prospectively. Event-free survival (EFS) was defined as time from diagnosis to progression or relapse, unplanned re-treatment after initial immunochemotherapy, or death from any cause. Overall survival (OS) was defined as time from diagnosis to death from any cause. Categorical data were analyzed by Chi-square test, and time-to-event data were analyzed using Kaplan-Meier method. Statistical analysis was done in SPSS (V22).
Results
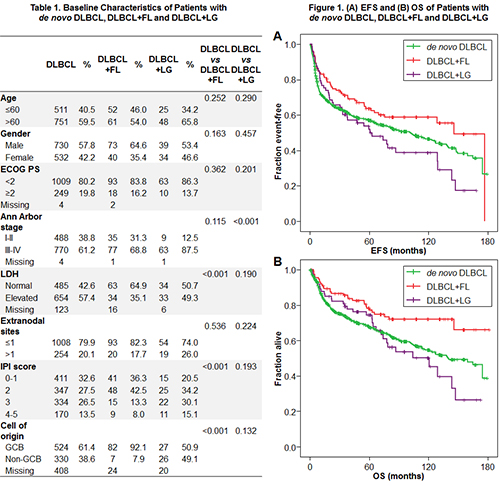
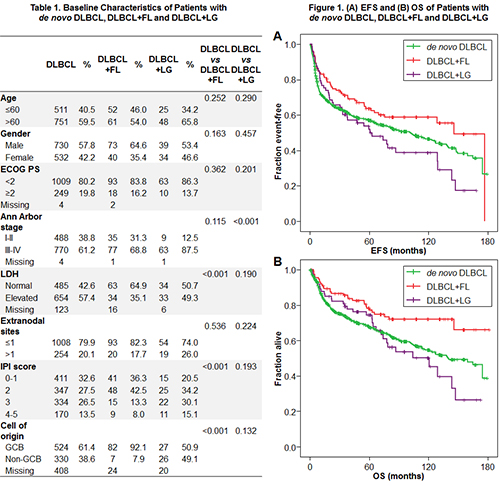
Among the 1448 patients, 1262 (87.2%) had de novo DLBCL, 113 (7.8%) had DLBCL+FL, and 73 (5.0%) had DLBCL+LG. In the DLBCL+FL cohort, 87 (77%) patients had DLBCL and FL at the same site (composite histology) while 26 (23%) had FL at other sites (discordant histology). In the DLBCL+LG cohort, 16 (21.9%) had composite histology and 57 (78.1%) had discordant histology, predominantly in the bone marrow (55). LG histology included marginal zone lymphoma (18), chronic lymphocytic leukemia/small lymphocytic lymphoma (14) and lymphoplasmacytic lymphoma (4). Baseline characteristics were summarized in Table 1. Compared with de novo DLBCL patients, DLBCL+FL patients had less elevations in LDH and lower IPI scores, while DLBCL+LG patients had more advanced stages (all P<0.001). Cell of origin by Hans was predominantly GCB in DLBCL+FL (92.1% vs 61.4% in de novo DLBCL, P<0.001). The proportion of GCB subtypes in DLBCL+LG was similar to that in de novo DLBCL (50.9% vs 61.4%, P=0.132). The median follow-up was 83.9 months. DLBCL+FL patients had superior EFS (median 145.9 vs 101.9 months, EFS rate at 24 months [EFS24] 74.5% vs 63.9%, P=0.049) and OS (median not reached vs 139.7 months, P=0.004) compared with de novo DLBCL patients (Figure 1). DLBCL+LG patients had similar EFS (median 63.0 vs 101.9 months, EFS24 65.8% vs 63.9%, P=0.269) and OS (median 120.7 vs 139.7 months, P=0.624) compared with de novo DLBCL patients. Relapses with DLBCL or FL/LG were equally common in DLBCL+FL (7 relapses with DLBCL, 7 with FL, 6 with both) and DLBCL+LG patients (12 relapses with DLBCL, 12 with LG, 3 with both).
Conclusion
Compared with de novo DLBCL patients, those with DLBCL+FL at diagnosis had predominantly GCB subtype of DLBCL, lower IPI scores, and improved EFS, EFS24 and OS, while those with DLBCL+LG had more advanced stages and similar outcomes. In DLBCL+FL and DLBCL+LG patients, relapses with DLBCL and FL or LG were equally common. DLBCL+FL likely behaves like GCB DLBCL, and this should be taken into consideration when including DLBCL+FL patients in DLBCL trials.
Session topic: 21. Aggressive Non-Hodgkin lymphoma - Clinical
Keyword(s): DLBCL, Follicular lymphoma, Low-grade NHL
Abstract: S1547
Type: Oral Presentation
Presentation during EHA23: On Sunday, June 17, 2018 from 08:30 - 08:45
Location: Room A1
Background
A significant percentage of patients with newly diagnosed diffuse large B-cell lymphoma (DLBCL) have concurrent follicular lymphoma (FL) or other low-grade B-cell lymphoma in tissue and/or bone marrow biopsies. Clinically these patients are usually treated in the same way as those with pure de novo DLBCL. However, it is unclear whether they also have identical outcomes compared with de novo DLBCL patients. As a result, whether to include these patients in clinical trials of DLBCL remains controversial.
Aims
To compare the clinical characteristics and outcomes of patients with de novo DLBCL, concurrent DLBCL and FL (DLBCL+FL), or concurrent DLBCL and other low-grade B-cell lymphoma (DLBCL+LG).
Methods
1448 patients with newly diagnosed DLBCL from March 2002 to April 2015 were included in this study. Patients were enrolled in the Molecular Epidemiology Resource (MER) of the University of Iowa/Mayo Clinic lymphoma Specialized Program of Research Excellence (SPORE), treated with standard immunochemotherapy and followed prospectively. Event-free survival (EFS) was defined as time from diagnosis to progression or relapse, unplanned re-treatment after initial immunochemotherapy, or death from any cause. Overall survival (OS) was defined as time from diagnosis to death from any cause. Categorical data were analyzed by Chi-square test, and time-to-event data were analyzed using Kaplan-Meier method. Statistical analysis was done in SPSS (V22).
Results
Among the 1448 patients, 1262 (87.2%) had de novo DLBCL, 113 (7.8%) had DLBCL+FL, and 73 (5.0%) had DLBCL+LG. In the DLBCL+FL cohort, 87 (77%) patients had DLBCL and FL at the same site (composite histology) while 26 (23%) had FL at other sites (discordant histology). In the DLBCL+LG cohort, 16 (21.9%) had composite histology and 57 (78.1%) had discordant histology, predominantly in the bone marrow (55). LG histology included marginal zone lymphoma (18), chronic lymphocytic leukemia/small lymphocytic lymphoma (14) and lymphoplasmacytic lymphoma (4). Baseline characteristics were summarized in Table 1. Compared with de novo DLBCL patients, DLBCL+FL patients had less elevations in LDH and lower IPI scores, while DLBCL+LG patients had more advanced stages (all P<0.001). Cell of origin by Hans was predominantly GCB in DLBCL+FL (92.1% vs 61.4% in de novo DLBCL, P<0.001). The proportion of GCB subtypes in DLBCL+LG was similar to that in de novo DLBCL (50.9% vs 61.4%, P=0.132). The median follow-up was 83.9 months. DLBCL+FL patients had superior EFS (median 145.9 vs 101.9 months, EFS rate at 24 months [EFS24] 74.5% vs 63.9%, P=0.049) and OS (median not reached vs 139.7 months, P=0.004) compared with de novo DLBCL patients (Figure 1). DLBCL+LG patients had similar EFS (median 63.0 vs 101.9 months, EFS24 65.8% vs 63.9%, P=0.269) and OS (median 120.7 vs 139.7 months, P=0.624) compared with de novo DLBCL patients. Relapses with DLBCL or FL/LG were equally common in DLBCL+FL (7 relapses with DLBCL, 7 with FL, 6 with both) and DLBCL+LG patients (12 relapses with DLBCL, 12 with LG, 3 with both).
Conclusion
Compared with de novo DLBCL patients, those with DLBCL+FL at diagnosis had predominantly GCB subtype of DLBCL, lower IPI scores, and improved EFS, EFS24 and OS, while those with DLBCL+LG had more advanced stages and similar outcomes. In DLBCL+FL and DLBCL+LG patients, relapses with DLBCL and FL or LG were equally common. DLBCL+FL likely behaves like GCB DLBCL, and this should be taken into consideration when including DLBCL+FL patients in DLBCL trials.
Session topic: 21. Aggressive Non-Hodgkin lymphoma - Clinical
Keyword(s): DLBCL, Follicular lymphoma, Low-grade NHL


