
Contributions
Abstract: S822
Type: Oral Presentation
Presentation during EHA23: On Saturday, June 16, 2018 from 12:30 - 12:45
Location: Room K1
Background
Clonal hematopoiesis of indeterminate potential (CHIP) occurs in the peripheral blood of approx. 20% of people > 60 years of age without history of hematologic disorders. CHIP associates with an increased risk of hematologic cancer, atherosclerotic disease and shorter overall survival. Case reports indicate that donor CHIP may lead to donor cell leukemia in the recipient. Collectively, these data might raise worries about the eligibility of a stem cell donor with CHIP.
Aims
We performed a comprehensive investigation to elucidate how donor CHIP - transferred from the donor to the recipient - affects the outcome of allogeneic hematopoietic stem cell transplantation (HSCT).
Methods
We included PB or BM samples from 488 healthy HSCT donors aged ≥ 55 years (median 63y) collected prior to or at the time of donation. Whole blood DNA was subjected to targeted sequencing using a 60-gene panel. Clinical data from the 488 transplant recipients were collected using a standardized catalogue of HSCT outcome parameters. AML was the most frequent diagnosis leading to HSCT (n=239), followed by MPN (n=55), MDS (n=53), multiple myeloma (n=41), lymphoma (n=40), ALL (n=24), and CLL (n=18). Due to their elevated age, the majority of donors were related to the recipient (98.6 %).
Results
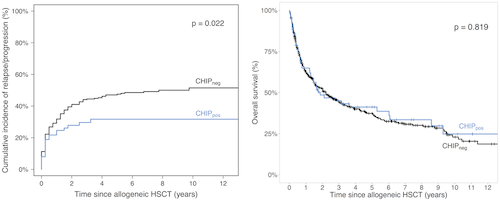
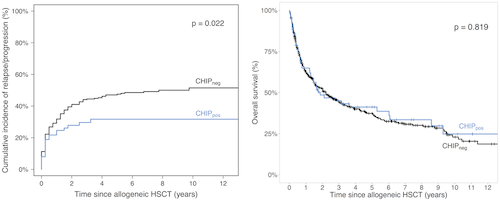
We identified 89 clonal mutations in 77/488 elderly donors (15.8%). The median VAF was 6.1% (range 2–43.0%) with 24 variants in 18 donors being present at a VAF ≥ 10%. 67 donors harbored one single CHIP mutation. Most frequently mutated genes were DNMT3A (37/488; 7.6%), TET2 (2.3%), ASXL1 (1.4%), SF3B1 and SRSF2 (0.8% each). Donor CHIP status was evenly distributed when looking at demographic, disease and transplantation characteristics of the recipient. Transplant failure, aGvHD and CMV reactivation were not affected by donor CHIP status, but cGvHD was significantly more often after HSCT with donor CHIP (54% vs. 39%; p=.018). Multivariate analysis confirmed donor CHIP as an independent risk factor for cGvHD (OR=1.8, 95% CI=1.05–2.95; p=.032). This was mainly attributed to DNMT3A mutations, which were associated with cGvHD in 64% of recipients (p=.004). Competing risk analysis identified donor CHIP to be associated with lower cumulative incidence of relapse/progression (CIR/P) in the recipient (p=.022) while non-relapse mortality was similar. Risk reduction was predominantly observed in recipients allografted in non-CR (n=297). Multivariate analysis confirmed donor CHIP as an independent risk factor for decreased CIR/P together with AML, cGvHD, CMV reactivation, donor age, ECOG performance and disease remission status (Fine and Gray test: HR=0.58; 95% CI=0.36–0.94; p=.029) in the entire cohort and in the subgroup of patients transplanted in non-CR (HR=0.36; 95%>CI = 0.151–0.842; p=.019). With respect to OS (median follow-up time for patients alive: 3.3y), neither donor CHIP status nor any single gene mutation affected survival, except for the MPN subgroup. MPN patients allografted with a clonal mutation (n=14) showed a reduced OS (p=.026). Serial quantification of 14 donor mutations in 50 follow-up samples suggests disproportionate expansion in most cases.
Conclusion
Allogeneic HSCT from a donor with CHIP appears safe and results in similar OS in the setting of elderly and related donors. Surprisingly, donor CHIP may increase cGvHD rates and reduce relapse/ progression risks. Future studies in younger and unrelated donors are warranted to confirm these results.
Session topic: 23. Stem cell transplantation - Clinical
Keyword(s): Allogeneic stem cell transplant, Clonality, Graft-versus-host disease (GVHD)
Abstract: S822
Type: Oral Presentation
Presentation during EHA23: On Saturday, June 16, 2018 from 12:30 - 12:45
Location: Room K1
Background
Clonal hematopoiesis of indeterminate potential (CHIP) occurs in the peripheral blood of approx. 20% of people > 60 years of age without history of hematologic disorders. CHIP associates with an increased risk of hematologic cancer, atherosclerotic disease and shorter overall survival. Case reports indicate that donor CHIP may lead to donor cell leukemia in the recipient. Collectively, these data might raise worries about the eligibility of a stem cell donor with CHIP.
Aims
We performed a comprehensive investigation to elucidate how donor CHIP - transferred from the donor to the recipient - affects the outcome of allogeneic hematopoietic stem cell transplantation (HSCT).
Methods
We included PB or BM samples from 488 healthy HSCT donors aged ≥ 55 years (median 63y) collected prior to or at the time of donation. Whole blood DNA was subjected to targeted sequencing using a 60-gene panel. Clinical data from the 488 transplant recipients were collected using a standardized catalogue of HSCT outcome parameters. AML was the most frequent diagnosis leading to HSCT (n=239), followed by MPN (n=55), MDS (n=53), multiple myeloma (n=41), lymphoma (n=40), ALL (n=24), and CLL (n=18). Due to their elevated age, the majority of donors were related to the recipient (98.6 %).
Results
We identified 89 clonal mutations in 77/488 elderly donors (15.8%). The median VAF was 6.1% (range 2–43.0%) with 24 variants in 18 donors being present at a VAF ≥ 10%. 67 donors harbored one single CHIP mutation. Most frequently mutated genes were DNMT3A (37/488; 7.6%), TET2 (2.3%), ASXL1 (1.4%), SF3B1 and SRSF2 (0.8% each). Donor CHIP status was evenly distributed when looking at demographic, disease and transplantation characteristics of the recipient. Transplant failure, aGvHD and CMV reactivation were not affected by donor CHIP status, but cGvHD was significantly more often after HSCT with donor CHIP (54% vs. 39%; p=.018). Multivariate analysis confirmed donor CHIP as an independent risk factor for cGvHD (OR=1.8, 95% CI=1.05–2.95; p=.032). This was mainly attributed to DNMT3A mutations, which were associated with cGvHD in 64% of recipients (p=.004). Competing risk analysis identified donor CHIP to be associated with lower cumulative incidence of relapse/progression (CIR/P) in the recipient (p=.022) while non-relapse mortality was similar. Risk reduction was predominantly observed in recipients allografted in non-CR (n=297). Multivariate analysis confirmed donor CHIP as an independent risk factor for decreased CIR/P together with AML, cGvHD, CMV reactivation, donor age, ECOG performance and disease remission status (Fine and Gray test: HR=0.58; 95% CI=0.36–0.94; p=.029) in the entire cohort and in the subgroup of patients transplanted in non-CR (HR=0.36; 95%>CI = 0.151–0.842; p=.019). With respect to OS (median follow-up time for patients alive: 3.3y), neither donor CHIP status nor any single gene mutation affected survival, except for the MPN subgroup. MPN patients allografted with a clonal mutation (n=14) showed a reduced OS (p=.026). Serial quantification of 14 donor mutations in 50 follow-up samples suggests disproportionate expansion in most cases.
Conclusion
Allogeneic HSCT from a donor with CHIP appears safe and results in similar OS in the setting of elderly and related donors. Surprisingly, donor CHIP may increase cGvHD rates and reduce relapse/ progression risks. Future studies in younger and unrelated donors are warranted to confirm these results.
Session topic: 23. Stem cell transplantation - Clinical
Keyword(s): Allogeneic stem cell transplant, Clonality, Graft-versus-host disease (GVHD)


