
Contributions
Abstract: S875
Type: Oral Presentation
Presentation during EHA23: On Saturday, June 16, 2018 from 17:00 - 17:15
Location: Room A6
Background
Allogeneic stem cell transplantation for peripheral T-cell lymphomas: a study of 284 patients from the Société Francophone de Greffe de Moelle et de Thérapie Cellulaire.
Aims
The aim of the current study was to analyse the outcomes ( overall survival, relpase/progression, non relapse mortality) in a cohort of patients who underwent an allo-HSCT for peripheral T cell lymphoma.
Methods
Based on the SFGM-TC database and on clinical files, we performed a retrospective multicentric analysis of adult patients who underwent an allo-SCT for non cutaneous PTCL between 2006 and 2014 in 34 centers. Primary cutaneous T cell lymphomas were excluded.
Results
A total of 284 patients with PTCL (NOS-T cell lymphomas: 39%, angioimmunoblastic T lymphomas: 29%, anaplastic T cell lymphomas 15%, others: 17%) were allo-transplanted in a median time of 12.6 months after diagnosis (3-322). Median age at transplant was 50 years (15 to 60 ) and 67% were males. At the time of transplant, 62% were in complete remission (CR), 27% in partial response (PR) and 11% in progressive disease (PD). Twenty-eight percent were transplanted in front line treatment, 36% after 2 lines of treatment and 35% after 3 or more lines of treatment; 23% had relapsed after a first autologous HSCT. Karnofsky index was up to 80% in 94% of the patients.
Donors were matched related in 45%, matched unrelated in 36% and alternative in 19% (haplo-identical n=7, cord blood n=33, mismatched 9/10 n=13) and SC source was peripheral blood in 71% of the patients.
Reduced intensity regiment was given in 147 patients (52%), myeloablative in 106 (38%) and non myeloablative (NMA) in 27 (10%). Fifty percent of the patient received an ex-vivo T cell depletion (ATG) whereas only 1% had an ex vivo T -depletion.
Fourteen patients (14%) developed grade III-IV acute GvHd, and 34% developed chronic GvHd (extensive for 13%).
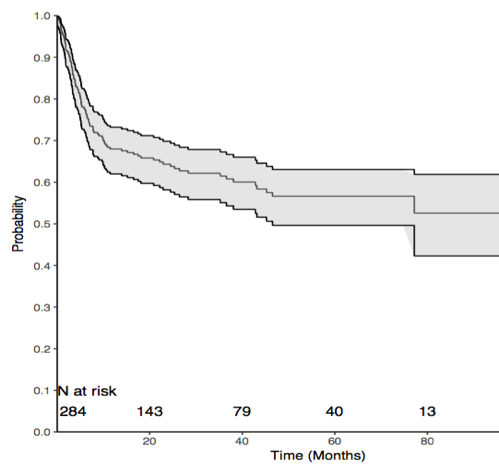
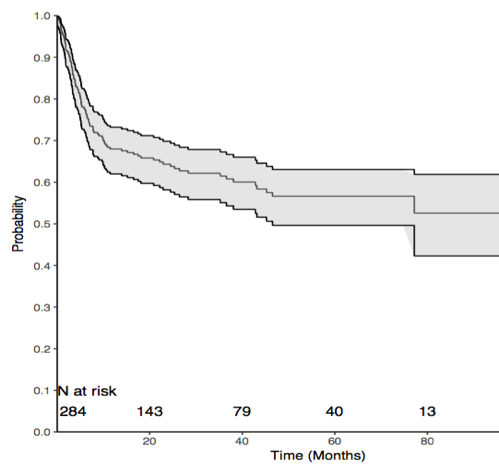
Median follow up was 33 months. One and 2 year -OS were 68% (95% 0.62-0.73) and 64% ( 95% 0.58-07). Cumulative incidence (CI) of relapse was 18% at 1 year and 22% at 2 years. The median time from transplant to relapse was 94 days and only 10% of the relapse occurred after the first year post transplant. Non relapse mortality (NRM) was 22% at 1 year and 24% at 2 years. The main causes of death were relapse (35%), infection (27%) or GvHD (22%).
In multivariate analysis, 5 year OS was significantly adversely influenced by the occurrence of grade III-IV aGvhd (HR: 2.52 (1.52-4.19), p< 0.01), low karnofsky score at the time of transplant (HR 2.22 (1.32-3.71), p: 0.002), cord blood transplant compared to bone marrow (HR 2.01 (1.00-4.01), p:0.049) . The main factor associated with NRM were patient’s age ( HR:1.02, p:0.084[MTR3] ) a low Karnofsky score (HR 2.03 (1.08-3.83) p: 0.029), female donor to male recipient (HR:1.87 (1.07-3.28), p: 0.027). The conditioning regimen intensity (RIC or MAC) was not found to have impact on OS. Among thirty patients transplanted in PD, 50% reached CR after allo-HSCT and 2 year-OS was 51% in this subgroup.
Figure: Overall survival for the 284 allo-HSCT for non cutaneous T-cell Lymphoma.
Conclusion
This is to our knowledge the largest cohort of allo-HSCT patients for T cell lymphoma, showing encouraging results in both MAC and RIC.
Session topic: 23. Stem cell transplantation - Clinical
Abstract: S875
Type: Oral Presentation
Presentation during EHA23: On Saturday, June 16, 2018 from 17:00 - 17:15
Location: Room A6
Background
Allogeneic stem cell transplantation for peripheral T-cell lymphomas: a study of 284 patients from the Société Francophone de Greffe de Moelle et de Thérapie Cellulaire.
Aims
The aim of the current study was to analyse the outcomes ( overall survival, relpase/progression, non relapse mortality) in a cohort of patients who underwent an allo-HSCT for peripheral T cell lymphoma.
Methods
Based on the SFGM-TC database and on clinical files, we performed a retrospective multicentric analysis of adult patients who underwent an allo-SCT for non cutaneous PTCL between 2006 and 2014 in 34 centers. Primary cutaneous T cell lymphomas were excluded.
Results
A total of 284 patients with PTCL (NOS-T cell lymphomas: 39%, angioimmunoblastic T lymphomas: 29%, anaplastic T cell lymphomas 15%, others: 17%) were allo-transplanted in a median time of 12.6 months after diagnosis (3-322). Median age at transplant was 50 years (15 to 60 ) and 67% were males. At the time of transplant, 62% were in complete remission (CR), 27% in partial response (PR) and 11% in progressive disease (PD). Twenty-eight percent were transplanted in front line treatment, 36% after 2 lines of treatment and 35% after 3 or more lines of treatment; 23% had relapsed after a first autologous HSCT. Karnofsky index was up to 80% in 94% of the patients.
Donors were matched related in 45%, matched unrelated in 36% and alternative in 19% (haplo-identical n=7, cord blood n=33, mismatched 9/10 n=13) and SC source was peripheral blood in 71% of the patients.
Reduced intensity regiment was given in 147 patients (52%), myeloablative in 106 (38%) and non myeloablative (NMA) in 27 (10%). Fifty percent of the patient received an ex-vivo T cell depletion (ATG) whereas only 1% had an ex vivo T -depletion.
Fourteen patients (14%) developed grade III-IV acute GvHd, and 34% developed chronic GvHd (extensive for 13%).
Median follow up was 33 months. One and 2 year -OS were 68% (95% 0.62-0.73) and 64% ( 95% 0.58-07). Cumulative incidence (CI) of relapse was 18% at 1 year and 22% at 2 years. The median time from transplant to relapse was 94 days and only 10% of the relapse occurred after the first year post transplant. Non relapse mortality (NRM) was 22% at 1 year and 24% at 2 years. The main causes of death were relapse (35%), infection (27%) or GvHD (22%).
In multivariate analysis, 5 year OS was significantly adversely influenced by the occurrence of grade III-IV aGvhd (HR: 2.52 (1.52-4.19), p< 0.01), low karnofsky score at the time of transplant (HR 2.22 (1.32-3.71), p: 0.002), cord blood transplant compared to bone marrow (HR 2.01 (1.00-4.01), p:0.049) . The main factor associated with NRM were patient’s age ( HR:1.02, p:0.084[MTR3] ) a low Karnofsky score (HR 2.03 (1.08-3.83) p: 0.029), female donor to male recipient (HR:1.87 (1.07-3.28), p: 0.027). The conditioning regimen intensity (RIC or MAC) was not found to have impact on OS. Among thirty patients transplanted in PD, 50% reached CR after allo-HSCT and 2 year-OS was 51% in this subgroup.
Figure: Overall survival for the 284 allo-HSCT for non cutaneous T-cell Lymphoma.
Conclusion
This is to our knowledge the largest cohort of allo-HSCT patients for T cell lymphoma, showing encouraging results in both MAC and RIC.
Session topic: 23. Stem cell transplantation - Clinical


