
Contributions
Abstract: PB2054
Type: Publication Only
Background
Aims
The purpose of this work is analyse the correlations between clinical-biological and histological characteristics of bone marrow biopsy and the mutational status (JAK2, CALR, MPL).
Methods
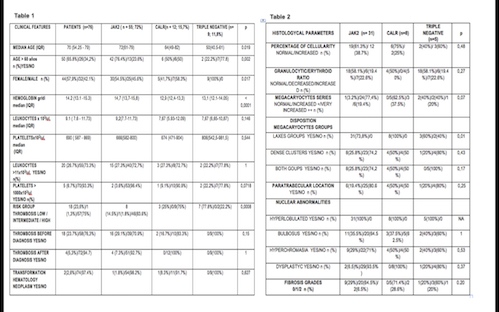
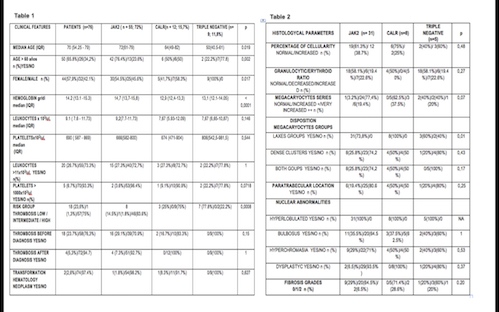
The study included 76 patients with ET diagnosed according to WHO criteria at the Haemathology Departament from Hospital de Jerez from January 2005 to December 2015. We examined the prevalence, and clinical and laboratory correlations of JAK2/CALR/MPL mutations. To evaluated the histology, one pathologist with expertise in haematopathology review the bone marrow biopsies corresponding to 44 patients with ET. We incluyed only bone marrow biopsies of at least 10 mm in length and/or minimun 8 inter-trabecular areas. The pathologist only had access to age and gender data. Mutations JAK, CALR and MPL were analysed by PCR real time and sanger sequencing.
Results
Conclusion
Session topic: 16. Myeloproliferative neoplasms - Clinical
Abstract: PB2054
Type: Publication Only
Background
Aims
The purpose of this work is analyse the correlations between clinical-biological and histological characteristics of bone marrow biopsy and the mutational status (JAK2, CALR, MPL).
Methods
The study included 76 patients with ET diagnosed according to WHO criteria at the Haemathology Departament from Hospital de Jerez from January 2005 to December 2015. We examined the prevalence, and clinical and laboratory correlations of JAK2/CALR/MPL mutations. To evaluated the histology, one pathologist with expertise in haematopathology review the bone marrow biopsies corresponding to 44 patients with ET. We incluyed only bone marrow biopsies of at least 10 mm in length and/or minimun 8 inter-trabecular areas. The pathologist only had access to age and gender data. Mutations JAK, CALR and MPL were analysed by PCR real time and sanger sequencing.
Results
Conclusion
Session topic: 16. Myeloproliferative neoplasms - Clinical


