
Contributions
Abstract: S802
Type: Oral Presentation
Presentation during EHA22: On Sunday, June 25, 2017 from 08:45 - 09:00
Location: Room N103
Background
Aims
Methods
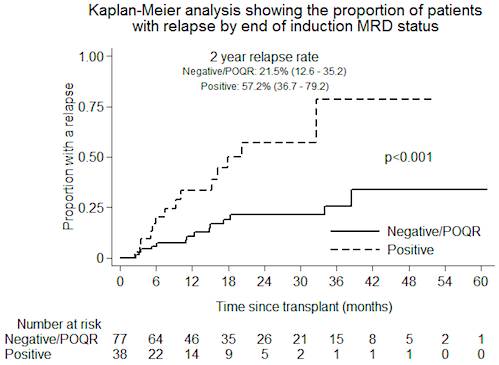
Results
| Patient characteristics | n=115 | Disease characteristics | n=115 |
| Age at randomisation median (range) | 49 (30-65) | B-ALL | 100 (87) |
| Presenting WBC median (range) | 8.6 (0.1-557) | T-ALL | 15 (13) |
| Sex N (%) | High-risk cytogenetics N (%) | ||
| Male | 61 (53) | BCR/ABL1 N (%) | 39 (33.9) |
| Female | 54 (47) | t(4,11) | 6 (5.2) |
| Donor type N (%) | Hypodiploidy/near triploidy | 7 (6.1) | |
| Sibling | 40 (34.8) | Complex karyotype | 3 (2.6) |
| Matched unrelated | 75 (65.2) | UKALL14 cytogenetic risk group N (%) | |
| Post induction MRD N (%) | Standard | 42 (36.5) | |
| Negative/POQR | 77 (67) | High risk | 53 (46.1) |
| Positive | 38 (33) | Unknown | 20 (17.4) |
Conclusion
Session topic: 2. Acute lymphoblastic leukemia - Clinical
Keyword(s): Reduced intensity transplantation, Minimal residual disease (MRD), Allogeneic hematopoietic stem cell transplant, Acute lymphoblastic leukemia
Abstract: S802
Type: Oral Presentation
Presentation during EHA22: On Sunday, June 25, 2017 from 08:45 - 09:00
Location: Room N103
Background
Aims
Methods
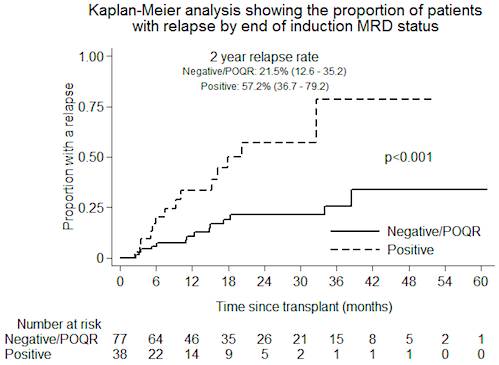
Results
| Patient characteristics | n=115 | Disease characteristics | n=115 |
| Age at randomisation median (range) | 49 (30-65) | B-ALL | 100 (87) |
| Presenting WBC median (range) | 8.6 (0.1-557) | T-ALL | 15 (13) |
| Sex N (%) | High-risk cytogenetics N (%) | ||
| Male | 61 (53) | BCR/ABL1 N (%) | 39 (33.9) |
| Female | 54 (47) | t(4,11) | 6 (5.2) |
| Donor type N (%) | Hypodiploidy/near triploidy | 7 (6.1) | |
| Sibling | 40 (34.8) | Complex karyotype | 3 (2.6) |
| Matched unrelated | 75 (65.2) | UKALL14 cytogenetic risk group N (%) | |
| Post induction MRD N (%) | Standard | 42 (36.5) | |
| Negative/POQR | 77 (67) | High risk | 53 (46.1) |
| Positive | 38 (33) | Unknown | 20 (17.4) |
Conclusion
Session topic: 2. Acute lymphoblastic leukemia - Clinical
Keyword(s): Reduced intensity transplantation, Minimal residual disease (MRD), Allogeneic hematopoietic stem cell transplant, Acute lymphoblastic leukemia


