
Contributions
Abstract: S452
Type: Oral Presentation
Presentation during EHA22: On Saturday, June 24, 2017 from 11:45 - 12:00
Location: Room N109
Background
Aims
The aim of this study was to make a worldwide inventory of all cases of PKD that have been treated by HSCT, and to evaluate indication, procedures employed, and outcome.
Methods
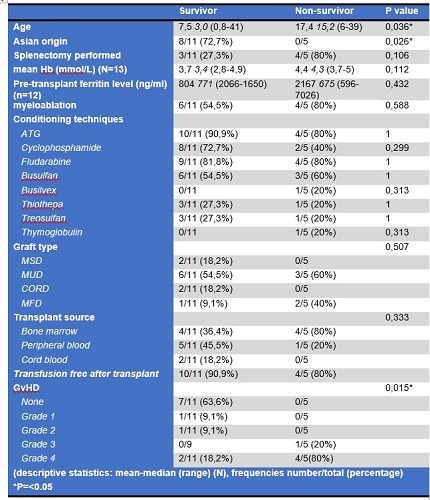
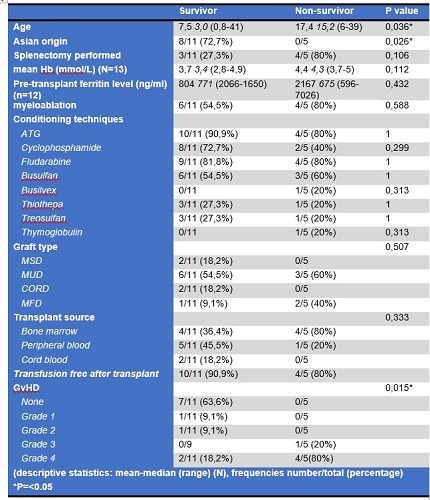
Results
Conclusion
This is the first study on outcome of HSCT in PKD patients. Due to the still relatively small number of cases no definite conclusions on the safety of HSCT in PKD can be drawn. However, we observed a better survival for patients transplanted before the age of ten. This difference could also explain difference in survival between patients transplanted in Europe versus Asia. The high rate of severe GvHD in this cohort is a reason for concern. The strong decline in survival of patients older than ten years of age indicates the need for very careful selection of HSCT-candidates.
Session topic: 27. Enzymopathies, membranopathies and other anemias
Keyword(s): Stem cell transplant, Hemolytic anemia, Treatment
Abstract: S452
Type: Oral Presentation
Presentation during EHA22: On Saturday, June 24, 2017 from 11:45 - 12:00
Location: Room N109
Background
Aims
The aim of this study was to make a worldwide inventory of all cases of PKD that have been treated by HSCT, and to evaluate indication, procedures employed, and outcome.
Methods
Results
Conclusion
This is the first study on outcome of HSCT in PKD patients. Due to the still relatively small number of cases no definite conclusions on the safety of HSCT in PKD can be drawn. However, we observed a better survival for patients transplanted before the age of ten. This difference could also explain difference in survival between patients transplanted in Europe versus Asia. The high rate of severe GvHD in this cohort is a reason for concern. The strong decline in survival of patients older than ten years of age indicates the need for very careful selection of HSCT-candidates.
Session topic: 27. Enzymopathies, membranopathies and other anemias
Keyword(s): Stem cell transplant, Hemolytic anemia, Treatment


