PHASE I/II STUDY OF VOSAROXIN AND DECITABINE IN NEWLY DIAGNOSED OLDER PATIENTS (PTS) WITH ACUTE MYELOID LEUKEMIA (AML) AND HIGH-RISK MYELODYSPLASTIC SYNDROME (MDS)
(Abstract release date: 05/19/16)
EHA Library. Daver N. 06/11/16; 135261; S505

Dr. Naval Daver
Contributions
Contributions
Abstract
Abstract: S505
Type: Oral Presentation
Presentation during EHA21: On Saturday, June 11, 2016 from 17:00 - 17:15
Location: Hall A3
Background
Vosaroxin, is a first-in-class anti-cancer quinolone derived (AQD) DNA topoisomerase II inhibitor currently under evaluation for the treatment of pts with AML and high-risk MDS.
Aims
To determine the overall response rate including complete response (CR) + CR without platelet recovery (CRp) + CR with insufficient hematological recovery (CRi), safety and early mortality of vosaroxin and decitabine in newly diagnosed older pts with AML.
Methods
Pts were eligible if they had untreated AML or high-risk MDS (≥ 10% blasts), were 60 years of age or older, had adequate performance status (ECOG ≤ 2) and organ function. In the phase I the first six pts received vosaroxin 90 mg/m2 daily on Days 1 and 4 with decitabine 20 mg/m2 daily for 5 days repeated in approximately 4 to 5 week intervals for up to 7 cycles. This dose was well tolerated in the 6 pts. However, due to occurrence of 8 episodes of grade 3/4 mucositis in the subsequent 16 pts the induction dose of vosaroxin was reduced to 70 mg/m2. 40 subsequent pts received vosaroxin 70mg/m2 in induction..
Results
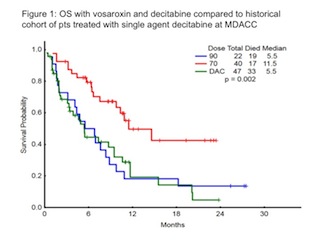
62 pts (55 AML, 7 high-risk MDS) with a median age of 69 years (range, 60 - 78) have been enrolled. They included 23 (37%) with diploid, 22 (35%) with adverse, and 17 (27%) pts with miscellaneous cytogenetics. 18 (33%) pts with AML had antecedent hematological disorders (AHD) including 9 (16%) with MDS, 5 (9%) with MDS/MPN, and 1 (2%) with CLL. Four pts with AHD had received prior therapy including 5-azacytidine (n=1), decitabine (n=1), ruxolitinib + 5-azacytidine (n=1), lenalidomide (n=1). Additionally, 10 (16%) pts had therapy-related disease. Median bone marrow blast %, median white blood cell, hemoglobin, & platelet counts were 36% (9-97), 3.6 x 109/L (0.4 - 57.0), 9.4 g/dL (6.8 - 13.1), and 33 x 109/L (7 - 333), respectively. All 62 pts were evaluable for response. The overall response rate was 74% including CR in 31 (50%), CRp in 10 (16%), and CRi in 5 (8%). Minimal residual disease by 19 color flow-cytometry was not detectable in 21 of 38 (55%) evaluable responders. The median number of cycles to response was 1 (1-4). Response by baseline characteristics is shown in table 1. Eleven (18%) pts have proceeded to allogeneic stem cell transplant. The median follow-up is 11.0 months (2.8 - 27.5). The main therapy related grade ≥ 3 toxicities were mucositis in 11 (18%) and liver enzyme elevation in 8 (13%) pts. The median overall survival (OS) for all pts is 9.8 months. Four-week and 8-week mortality for all pts were 0 and 13%, respectively. The induction dose of vosaroxin was 90 mg/m2 in 22 pts and 70 mg/m2 in 40 pts. The lower dose of vosaroxin was associated with reduced 8-week mortality (8% versus 23%), similar overall response (75% versus 73%), and improved OS (Fig 1).Table 1: Response by baseline characteristics
Conclusion
Combination of vosaroxin and decitabine is effective in older pts with AML and high-risk MDS. The lower dose of vosaroxin 70 mg/m2 on days 1 and 4 is associated with improved outcomes.
Session topic: New Compounds in AML Treatment
Keyword(s): AML, Decitabine, Elderly, Hypomethylation
Type: Oral Presentation
Presentation during EHA21: On Saturday, June 11, 2016 from 17:00 - 17:15
Location: Hall A3
Background
Vosaroxin, is a first-in-class anti-cancer quinolone derived (AQD) DNA topoisomerase II inhibitor currently under evaluation for the treatment of pts with AML and high-risk MDS.
Aims
To determine the overall response rate including complete response (CR) + CR without platelet recovery (CRp) + CR with insufficient hematological recovery (CRi), safety and early mortality of vosaroxin and decitabine in newly diagnosed older pts with AML.
Methods
Pts were eligible if they had untreated AML or high-risk MDS (≥ 10% blasts), were 60 years of age or older, had adequate performance status (ECOG ≤ 2) and organ function. In the phase I the first six pts received vosaroxin 90 mg/m2 daily on Days 1 and 4 with decitabine 20 mg/m2 daily for 5 days repeated in approximately 4 to 5 week intervals for up to 7 cycles. This dose was well tolerated in the 6 pts. However, due to occurrence of 8 episodes of grade 3/4 mucositis in the subsequent 16 pts the induction dose of vosaroxin was reduced to 70 mg/m2. 40 subsequent pts received vosaroxin 70mg/m2 in induction..
Results
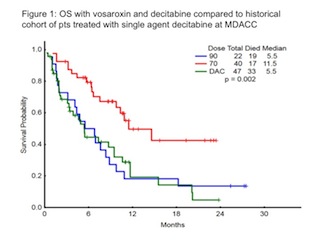
62 pts (55 AML, 7 high-risk MDS) with a median age of 69 years (range, 60 - 78) have been enrolled. They included 23 (37%) with diploid, 22 (35%) with adverse, and 17 (27%) pts with miscellaneous cytogenetics. 18 (33%) pts with AML had antecedent hematological disorders (AHD) including 9 (16%) with MDS, 5 (9%) with MDS/MPN, and 1 (2%) with CLL. Four pts with AHD had received prior therapy including 5-azacytidine (n=1), decitabine (n=1), ruxolitinib + 5-azacytidine (n=1), lenalidomide (n=1). Additionally, 10 (16%) pts had therapy-related disease. Median bone marrow blast %, median white blood cell, hemoglobin, & platelet counts were 36% (9-97), 3.6 x 109/L (0.4 - 57.0), 9.4 g/dL (6.8 - 13.1), and 33 x 109/L (7 - 333), respectively. All 62 pts were evaluable for response. The overall response rate was 74% including CR in 31 (50%), CRp in 10 (16%), and CRi in 5 (8%). Minimal residual disease by 19 color flow-cytometry was not detectable in 21 of 38 (55%) evaluable responders. The median number of cycles to response was 1 (1-4). Response by baseline characteristics is shown in table 1. Eleven (18%) pts have proceeded to allogeneic stem cell transplant. The median follow-up is 11.0 months (2.8 - 27.5). The main therapy related grade ≥ 3 toxicities were mucositis in 11 (18%) and liver enzyme elevation in 8 (13%) pts. The median overall survival (OS) for all pts is 9.8 months. Four-week and 8-week mortality for all pts were 0 and 13%, respectively. The induction dose of vosaroxin was 90 mg/m2 in 22 pts and 70 mg/m2 in 40 pts. The lower dose of vosaroxin was associated with reduced 8-week mortality (8% versus 23%), similar overall response (75% versus 73%), and improved OS (Fig 1).Table 1: Response by baseline characteristics
| Parameter | Category | N | Overall response(CR, CRp, CRi) | CR |
| Age | 60-74≥75 | 5012 | 74%75% | 52%42% |
| Cytogenetics | Diploid | 23 | 83% | 57% |
| -5/-7/other adverse | 22 | 64% | 36% | |
| Miscellaneous | 17 | 76% | 59% | |
| MutationStatus | TP53IDH2 | 1311 | 69%91% | 46%82% |
| IDH1 | 9 | 33% | 33% | |
| RAS | 11 | 64% | 18% |
Conclusion
Combination of vosaroxin and decitabine is effective in older pts with AML and high-risk MDS. The lower dose of vosaroxin 70 mg/m2 on days 1 and 4 is associated with improved outcomes.
Session topic: New Compounds in AML Treatment
Keyword(s): AML, Decitabine, Elderly, Hypomethylation
Abstract: S505
Type: Oral Presentation
Presentation during EHA21: On Saturday, June 11, 2016 from 17:00 - 17:15
Location: Hall A3
Background
Vosaroxin, is a first-in-class anti-cancer quinolone derived (AQD) DNA topoisomerase II inhibitor currently under evaluation for the treatment of pts with AML and high-risk MDS.
Aims
To determine the overall response rate including complete response (CR) + CR without platelet recovery (CRp) + CR with insufficient hematological recovery (CRi), safety and early mortality of vosaroxin and decitabine in newly diagnosed older pts with AML.
Methods
Pts were eligible if they had untreated AML or high-risk MDS (≥ 10% blasts), were 60 years of age or older, had adequate performance status (ECOG ≤ 2) and organ function. In the phase I the first six pts received vosaroxin 90 mg/m2 daily on Days 1 and 4 with decitabine 20 mg/m2 daily for 5 days repeated in approximately 4 to 5 week intervals for up to 7 cycles. This dose was well tolerated in the 6 pts. However, due to occurrence of 8 episodes of grade 3/4 mucositis in the subsequent 16 pts the induction dose of vosaroxin was reduced to 70 mg/m2. 40 subsequent pts received vosaroxin 70mg/m2 in induction..
Results
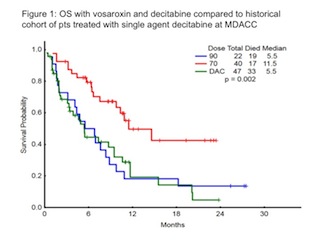
62 pts (55 AML, 7 high-risk MDS) with a median age of 69 years (range, 60 - 78) have been enrolled. They included 23 (37%) with diploid, 22 (35%) with adverse, and 17 (27%) pts with miscellaneous cytogenetics. 18 (33%) pts with AML had antecedent hematological disorders (AHD) including 9 (16%) with MDS, 5 (9%) with MDS/MPN, and 1 (2%) with CLL. Four pts with AHD had received prior therapy including 5-azacytidine (n=1), decitabine (n=1), ruxolitinib + 5-azacytidine (n=1), lenalidomide (n=1). Additionally, 10 (16%) pts had therapy-related disease. Median bone marrow blast %, median white blood cell, hemoglobin, & platelet counts were 36% (9-97), 3.6 x 109/L (0.4 - 57.0), 9.4 g/dL (6.8 - 13.1), and 33 x 109/L (7 - 333), respectively. All 62 pts were evaluable for response. The overall response rate was 74% including CR in 31 (50%), CRp in 10 (16%), and CRi in 5 (8%). Minimal residual disease by 19 color flow-cytometry was not detectable in 21 of 38 (55%) evaluable responders. The median number of cycles to response was 1 (1-4). Response by baseline characteristics is shown in table 1. Eleven (18%) pts have proceeded to allogeneic stem cell transplant. The median follow-up is 11.0 months (2.8 - 27.5). The main therapy related grade ≥ 3 toxicities were mucositis in 11 (18%) and liver enzyme elevation in 8 (13%) pts. The median overall survival (OS) for all pts is 9.8 months. Four-week and 8-week mortality for all pts were 0 and 13%, respectively. The induction dose of vosaroxin was 90 mg/m2 in 22 pts and 70 mg/m2 in 40 pts. The lower dose of vosaroxin was associated with reduced 8-week mortality (8% versus 23%), similar overall response (75% versus 73%), and improved OS (Fig 1).Table 1: Response by baseline characteristics
Conclusion
Combination of vosaroxin and decitabine is effective in older pts with AML and high-risk MDS. The lower dose of vosaroxin 70 mg/m2 on days 1 and 4 is associated with improved outcomes.
Session topic: New Compounds in AML Treatment
Keyword(s): AML, Decitabine, Elderly, Hypomethylation
Type: Oral Presentation
Presentation during EHA21: On Saturday, June 11, 2016 from 17:00 - 17:15
Location: Hall A3
Background
Vosaroxin, is a first-in-class anti-cancer quinolone derived (AQD) DNA topoisomerase II inhibitor currently under evaluation for the treatment of pts with AML and high-risk MDS.
Aims
To determine the overall response rate including complete response (CR) + CR without platelet recovery (CRp) + CR with insufficient hematological recovery (CRi), safety and early mortality of vosaroxin and decitabine in newly diagnosed older pts with AML.
Methods
Pts were eligible if they had untreated AML or high-risk MDS (≥ 10% blasts), were 60 years of age or older, had adequate performance status (ECOG ≤ 2) and organ function. In the phase I the first six pts received vosaroxin 90 mg/m2 daily on Days 1 and 4 with decitabine 20 mg/m2 daily for 5 days repeated in approximately 4 to 5 week intervals for up to 7 cycles. This dose was well tolerated in the 6 pts. However, due to occurrence of 8 episodes of grade 3/4 mucositis in the subsequent 16 pts the induction dose of vosaroxin was reduced to 70 mg/m2. 40 subsequent pts received vosaroxin 70mg/m2 in induction..
Results
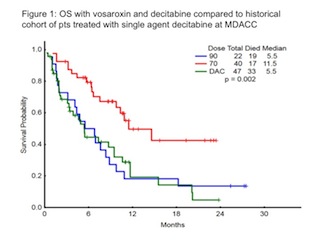
62 pts (55 AML, 7 high-risk MDS) with a median age of 69 years (range, 60 - 78) have been enrolled. They included 23 (37%) with diploid, 22 (35%) with adverse, and 17 (27%) pts with miscellaneous cytogenetics. 18 (33%) pts with AML had antecedent hematological disorders (AHD) including 9 (16%) with MDS, 5 (9%) with MDS/MPN, and 1 (2%) with CLL. Four pts with AHD had received prior therapy including 5-azacytidine (n=1), decitabine (n=1), ruxolitinib + 5-azacytidine (n=1), lenalidomide (n=1). Additionally, 10 (16%) pts had therapy-related disease. Median bone marrow blast %, median white blood cell, hemoglobin, & platelet counts were 36% (9-97), 3.6 x 109/L (0.4 - 57.0), 9.4 g/dL (6.8 - 13.1), and 33 x 109/L (7 - 333), respectively. All 62 pts were evaluable for response. The overall response rate was 74% including CR in 31 (50%), CRp in 10 (16%), and CRi in 5 (8%). Minimal residual disease by 19 color flow-cytometry was not detectable in 21 of 38 (55%) evaluable responders. The median number of cycles to response was 1 (1-4). Response by baseline characteristics is shown in table 1. Eleven (18%) pts have proceeded to allogeneic stem cell transplant. The median follow-up is 11.0 months (2.8 - 27.5). The main therapy related grade ≥ 3 toxicities were mucositis in 11 (18%) and liver enzyme elevation in 8 (13%) pts. The median overall survival (OS) for all pts is 9.8 months. Four-week and 8-week mortality for all pts were 0 and 13%, respectively. The induction dose of vosaroxin was 90 mg/m2 in 22 pts and 70 mg/m2 in 40 pts. The lower dose of vosaroxin was associated with reduced 8-week mortality (8% versus 23%), similar overall response (75% versus 73%), and improved OS (Fig 1).Table 1: Response by baseline characteristics
| Parameter | Category | N | Overall response(CR, CRp, CRi) | CR |
| Age | 60-74≥75 | 5012 | 74%75% | 52%42% |
| Cytogenetics | Diploid | 23 | 83% | 57% |
| -5/-7/other adverse | 22 | 64% | 36% | |
| Miscellaneous | 17 | 76% | 59% | |
| MutationStatus | TP53IDH2 | 1311 | 69%91% | 46%82% |
| IDH1 | 9 | 33% | 33% | |
| RAS | 11 | 64% | 18% |
Conclusion
Combination of vosaroxin and decitabine is effective in older pts with AML and high-risk MDS. The lower dose of vosaroxin 70 mg/m2 on days 1 and 4 is associated with improved outcomes.
Session topic: New Compounds in AML Treatment
Keyword(s): AML, Decitabine, Elderly, Hypomethylation
{{ help_message }}
{{filter}}


