ROUTINE IMAGING FOR PERIPHERAL T-CELL LYMPHOMA IN FIRST COMPLETE REMISSION DOES NOT IMPROVE SURVIVAL: A DANISH-SWEDISH POPULATION-BASED STUDY
(Abstract release date: 05/19/16)
EHA Library. Cederleuf H. 06/09/16; 132502; E953
Disclosure(s): Nothing.

Dr. Henrik Cederleuf
Contributions
Contributions
Abstract
Abstract: E953
Type: Eposter Presentation
Background
Routine surveillance imaging plays a limited role in detecting lymphoma relapse and a recent Danish-Swedish study showed that imaging-based follow-up practice was not associated with better outcome for diffuse large B-cell lymphoma (DLBCL) patients.
Aims
Using a similar approach, we evaluated the outcome of Danish and Swedish patients with nodal peripheral T-cell lymphoma (PTCL) in first CR for whom traditions for routine imaging have been different.
Methods
Patients from the Danish and Swedish lymphoma registries were selected by the following criteria: a) newly diagnosed nodal PTCL from 2007 to 2012, b) age ≥ 18 years, and c) CR after CHOP or CHOEP therapy with or without consolidating high-dose therapy (HDT). Follow-up for Swedish patients included symptom assessment, clinical examinations and blood tests at 3- to 4-month intervals for 2 years, with longer intervals later in follow-up. The national Swedish guidelines only recommended imaging when relapse was clinically suspected. Follow-up for Danish patients was similar but included routine imaging, usually computed tomography (CT) every 6 months for 2 years and at some centers annual CT from the 3rd till the 5th year of follow-up as well.
Results
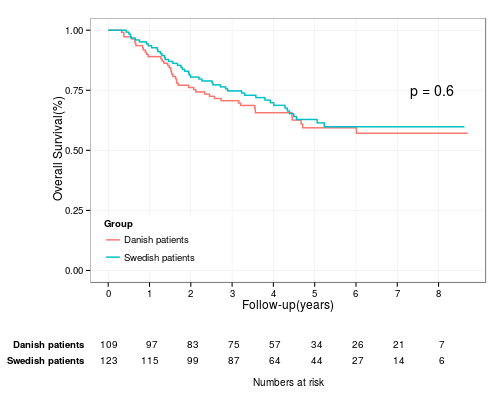
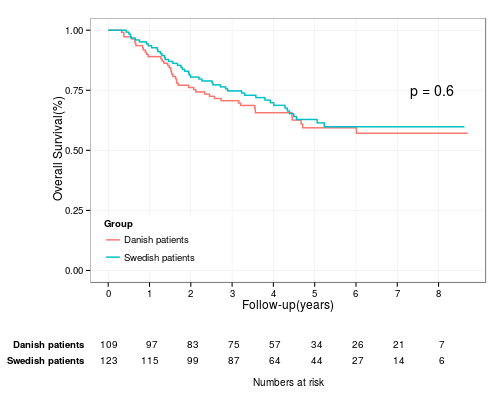
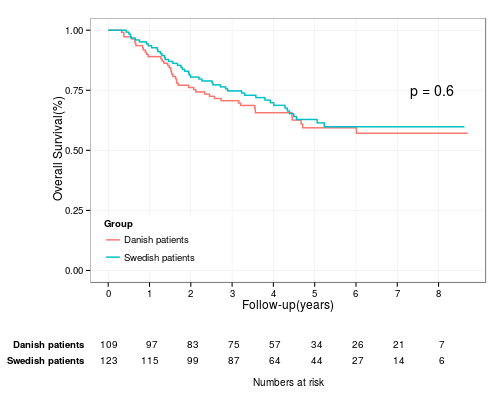
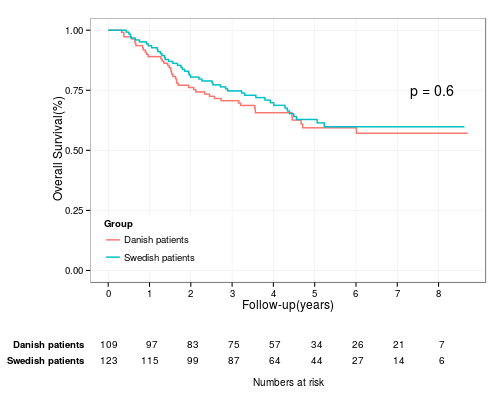
In total, 109 Danish patients and 123 Swedish patients with nodal PTCLs were included. PTCL not otherwise specified (NOS) was diagnosed in 95 patients, anaplastic large cell lymphoma (ALCL) in 88 patients, and angioimmunoblastic T-cell lymphoma (AITL) in 49 patients and with similar subtype frequencies for Danish and Swedish patients. The baseline demographic characteristics were also fully comparable between Danish and Swedish patients (Table 1). The OS estimates for Danish and Swedish patients in CR following frontline therapy were similar for all patients (P=0.6, Fig 1) and in PTCL subtype specific analyses. The most important adverse predictor of OS following CR was age > 60 (Hazard Ratio [HR], 3.73; 95 % CI, 2.08 to 6.66, P<0.01). The 2-year probability of relapse was similar for Danish and Swedish patients (25%; 95 % CI 16-33% vs. 29%; 95 % CI 19-38 %, P=0.53). The post-relapse OS was similar for Danish and Swedish patients overall (P=0.8) and in PTCL subtype specific analyses.
Table 1. Demographic and clinicopathological information on Danish and Swedish patients with nodal PTCL.
Conclusion
Relapse following frontline treatment for PTCL is typically associated with a poor prognosis and an imaging based follow-up practice did not translate into better survival for Danish patients. Thus, a follow-up strategy without routine surveillance imaging appears safe and equally effective to a FU strategy with imaging for patients with nodal PTCL in first CR.
Session topic: E-poster
Keyword(s): Peripheral T-cell lymphoma, Survival
Type: Eposter Presentation
Background
Routine surveillance imaging plays a limited role in detecting lymphoma relapse and a recent Danish-Swedish study showed that imaging-based follow-up practice was not associated with better outcome for diffuse large B-cell lymphoma (DLBCL) patients.
Aims
Using a similar approach, we evaluated the outcome of Danish and Swedish patients with nodal peripheral T-cell lymphoma (PTCL) in first CR for whom traditions for routine imaging have been different.
Methods
Patients from the Danish and Swedish lymphoma registries were selected by the following criteria: a) newly diagnosed nodal PTCL from 2007 to 2012, b) age ≥ 18 years, and c) CR after CHOP or CHOEP therapy with or without consolidating high-dose therapy (HDT). Follow-up for Swedish patients included symptom assessment, clinical examinations and blood tests at 3- to 4-month intervals for 2 years, with longer intervals later in follow-up. The national Swedish guidelines only recommended imaging when relapse was clinically suspected. Follow-up for Danish patients was similar but included routine imaging, usually computed tomography (CT) every 6 months for 2 years and at some centers annual CT from the 3rd till the 5th year of follow-up as well.
Results
In total, 109 Danish patients and 123 Swedish patients with nodal PTCLs were included. PTCL not otherwise specified (NOS) was diagnosed in 95 patients, anaplastic large cell lymphoma (ALCL) in 88 patients, and angioimmunoblastic T-cell lymphoma (AITL) in 49 patients and with similar subtype frequencies for Danish and Swedish patients. The baseline demographic characteristics were also fully comparable between Danish and Swedish patients (Table 1). The OS estimates for Danish and Swedish patients in CR following frontline therapy were similar for all patients (P=0.6, Fig 1) and in PTCL subtype specific analyses. The most important adverse predictor of OS following CR was age > 60 (Hazard Ratio [HR], 3.73; 95 % CI, 2.08 to 6.66, P<0.01). The 2-year probability of relapse was similar for Danish and Swedish patients (25%; 95 % CI 16-33% vs. 29%; 95 % CI 19-38 %, P=0.53). The post-relapse OS was similar for Danish and Swedish patients overall (P=0.8) and in PTCL subtype specific analyses.
| DK (n=109) | SWE (n=123) | Missing (DK/SWE) | P-value | |
| Median age (years) | 61 (21-89) | 64 (20-87) | 0/0 | 0.29 |
| Male-female ratio | 1.27 | 1.51 | 0/0 | 0.59 |
| IPI > 2, n (%) | 31 (29.8) | 36 (30.0) | 5/3 | 1.00 |
| ECOG >= 2 | 14 (13.0) | 16 (13.2) | 1/2 | 1.00 |
| Induction chemo CHOP | 77 (70.6) | 72 (58.5) | 0/0 | 0.07 |
| Induction chemo CHOEP | 32 (29.4) | 51 (41.5) | 0/0 | 0.07 |
| ALCL | 42 (39) | 46 (37) | 0/0 | 0.33 |
| AITL | 27 (25) | 22 (18) | 0/0 | 0.33 |
| PTCL NOS | 40 (37) | 55 (45) | 0/0 | 0.33 |
Conclusion
Relapse following frontline treatment for PTCL is typically associated with a poor prognosis and an imaging based follow-up practice did not translate into better survival for Danish patients. Thus, a follow-up strategy without routine surveillance imaging appears safe and equally effective to a FU strategy with imaging for patients with nodal PTCL in first CR.
Session topic: E-poster
Keyword(s): Peripheral T-cell lymphoma, Survival
Abstract: E953
Type: Eposter Presentation
Background
Routine surveillance imaging plays a limited role in detecting lymphoma relapse and a recent Danish-Swedish study showed that imaging-based follow-up practice was not associated with better outcome for diffuse large B-cell lymphoma (DLBCL) patients.
Aims
Using a similar approach, we evaluated the outcome of Danish and Swedish patients with nodal peripheral T-cell lymphoma (PTCL) in first CR for whom traditions for routine imaging have been different.
Methods
Patients from the Danish and Swedish lymphoma registries were selected by the following criteria: a) newly diagnosed nodal PTCL from 2007 to 2012, b) age ≥ 18 years, and c) CR after CHOP or CHOEP therapy with or without consolidating high-dose therapy (HDT). Follow-up for Swedish patients included symptom assessment, clinical examinations and blood tests at 3- to 4-month intervals for 2 years, with longer intervals later in follow-up. The national Swedish guidelines only recommended imaging when relapse was clinically suspected. Follow-up for Danish patients was similar but included routine imaging, usually computed tomography (CT) every 6 months for 2 years and at some centers annual CT from the 3rd till the 5th year of follow-up as well.
Results
In total, 109 Danish patients and 123 Swedish patients with nodal PTCLs were included. PTCL not otherwise specified (NOS) was diagnosed in 95 patients, anaplastic large cell lymphoma (ALCL) in 88 patients, and angioimmunoblastic T-cell lymphoma (AITL) in 49 patients and with similar subtype frequencies for Danish and Swedish patients. The baseline demographic characteristics were also fully comparable between Danish and Swedish patients (Table 1). The OS estimates for Danish and Swedish patients in CR following frontline therapy were similar for all patients (P=0.6, Fig 1) and in PTCL subtype specific analyses. The most important adverse predictor of OS following CR was age > 60 (Hazard Ratio [HR], 3.73; 95 % CI, 2.08 to 6.66, P<0.01). The 2-year probability of relapse was similar for Danish and Swedish patients (25%; 95 % CI 16-33% vs. 29%; 95 % CI 19-38 %, P=0.53). The post-relapse OS was similar for Danish and Swedish patients overall (P=0.8) and in PTCL subtype specific analyses.
Table 1. Demographic and clinicopathological information on Danish and Swedish patients with nodal PTCL.
Conclusion
Relapse following frontline treatment for PTCL is typically associated with a poor prognosis and an imaging based follow-up practice did not translate into better survival for Danish patients. Thus, a follow-up strategy without routine surveillance imaging appears safe and equally effective to a FU strategy with imaging for patients with nodal PTCL in first CR.
Session topic: E-poster
Keyword(s): Peripheral T-cell lymphoma, Survival
Type: Eposter Presentation
Background
Routine surveillance imaging plays a limited role in detecting lymphoma relapse and a recent Danish-Swedish study showed that imaging-based follow-up practice was not associated with better outcome for diffuse large B-cell lymphoma (DLBCL) patients.
Aims
Using a similar approach, we evaluated the outcome of Danish and Swedish patients with nodal peripheral T-cell lymphoma (PTCL) in first CR for whom traditions for routine imaging have been different.
Methods
Patients from the Danish and Swedish lymphoma registries were selected by the following criteria: a) newly diagnosed nodal PTCL from 2007 to 2012, b) age ≥ 18 years, and c) CR after CHOP or CHOEP therapy with or without consolidating high-dose therapy (HDT). Follow-up for Swedish patients included symptom assessment, clinical examinations and blood tests at 3- to 4-month intervals for 2 years, with longer intervals later in follow-up. The national Swedish guidelines only recommended imaging when relapse was clinically suspected. Follow-up for Danish patients was similar but included routine imaging, usually computed tomography (CT) every 6 months for 2 years and at some centers annual CT from the 3rd till the 5th year of follow-up as well.
Results
In total, 109 Danish patients and 123 Swedish patients with nodal PTCLs were included. PTCL not otherwise specified (NOS) was diagnosed in 95 patients, anaplastic large cell lymphoma (ALCL) in 88 patients, and angioimmunoblastic T-cell lymphoma (AITL) in 49 patients and with similar subtype frequencies for Danish and Swedish patients. The baseline demographic characteristics were also fully comparable between Danish and Swedish patients (Table 1). The OS estimates for Danish and Swedish patients in CR following frontline therapy were similar for all patients (P=0.6, Fig 1) and in PTCL subtype specific analyses. The most important adverse predictor of OS following CR was age > 60 (Hazard Ratio [HR], 3.73; 95 % CI, 2.08 to 6.66, P<0.01). The 2-year probability of relapse was similar for Danish and Swedish patients (25%; 95 % CI 16-33% vs. 29%; 95 % CI 19-38 %, P=0.53). The post-relapse OS was similar for Danish and Swedish patients overall (P=0.8) and in PTCL subtype specific analyses.
| DK (n=109) | SWE (n=123) | Missing (DK/SWE) | P-value | |
| Median age (years) | 61 (21-89) | 64 (20-87) | 0/0 | 0.29 |
| Male-female ratio | 1.27 | 1.51 | 0/0 | 0.59 |
| IPI > 2, n (%) | 31 (29.8) | 36 (30.0) | 5/3 | 1.00 |
| ECOG >= 2 | 14 (13.0) | 16 (13.2) | 1/2 | 1.00 |
| Induction chemo CHOP | 77 (70.6) | 72 (58.5) | 0/0 | 0.07 |
| Induction chemo CHOEP | 32 (29.4) | 51 (41.5) | 0/0 | 0.07 |
| ALCL | 42 (39) | 46 (37) | 0/0 | 0.33 |
| AITL | 27 (25) | 22 (18) | 0/0 | 0.33 |
| PTCL NOS | 40 (37) | 55 (45) | 0/0 | 0.33 |
Conclusion
Relapse following frontline treatment for PTCL is typically associated with a poor prognosis and an imaging based follow-up practice did not translate into better survival for Danish patients. Thus, a follow-up strategy without routine surveillance imaging appears safe and equally effective to a FU strategy with imaging for patients with nodal PTCL in first CR.
Session topic: E-poster
Keyword(s): Peripheral T-cell lymphoma, Survival
{{ help_message }}
{{filter}}


