UNRELATED DONOR (UD) ALLOGENEIC STEM CELL TRANSPLANTATION (ALLO-SCT) IN PRIMARY REFRACTORY ACUTE MYELOID LEUKEMIA (AML): REPORT OF 381 PATIENTS FROM THE ACUTE LEUKEMIA WORKING PARTY OF EBMT
(Abstract release date: 05/21/15)
EHA Library. Brissot E. 06/12/15; 103119; S128
Disclosure(s): Service d’Hématologie Clinique et de Thérapie Cellulaire, Hôpital Saint Antoine, APHP, Paris, FranceHematologie

Eolia Brissot
Contributions
Contributions
Abstract
Abstract: S128
Type: Oral Presentation
Presentation during EHA20: From 12.06.2015 12:00 to 12.06.2015 12:15
Location: Room Lehar 1 + 2
Background
Primary refractory AML is associated with a dismal prognosis. Approximately one third of patients younger than 60 years, and 50 % of older patients, with newly diagnosed AML fail to achieve complete remission (CR) with standard induction chemotherapy. Allo-SCT in the setting of active disease is an alternative but highly debatable strategy. The increased availability of UD and the use of reduced-intensity conditioning (RIC) regimens have opened the possibility for transplantation to a larger number of patients in comparison to standard myeloablative regimens (MAC)
Aims
The current study aimed to assess outcomes in a cohort of 381 primary refractory AML patients who received allo-SCT from an UD (10/10 or 9/10). Primary refractoriness was defined as failure to achieve CR within 60 days after starting induction.
Methods
Patients with primary refractory AML reported between 2000 and 2013 to the registry of the Acute Leukemia Working Party of the EBMT were included in this study. The major endpoints were to assess overall survival (OS), leukemia-free survival (LFS), relapse incidence (RI), and non relapse mortality (NRM).
Results
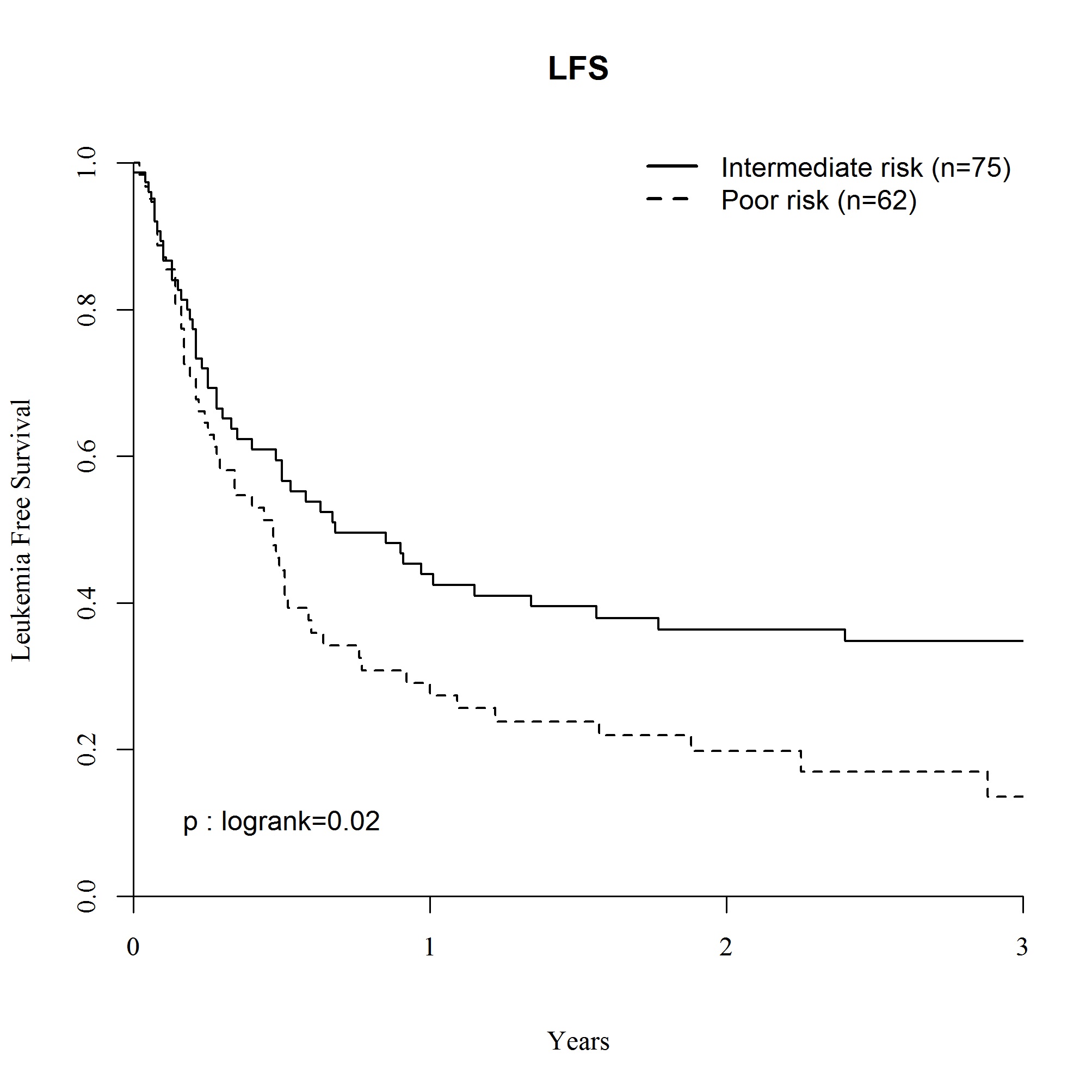
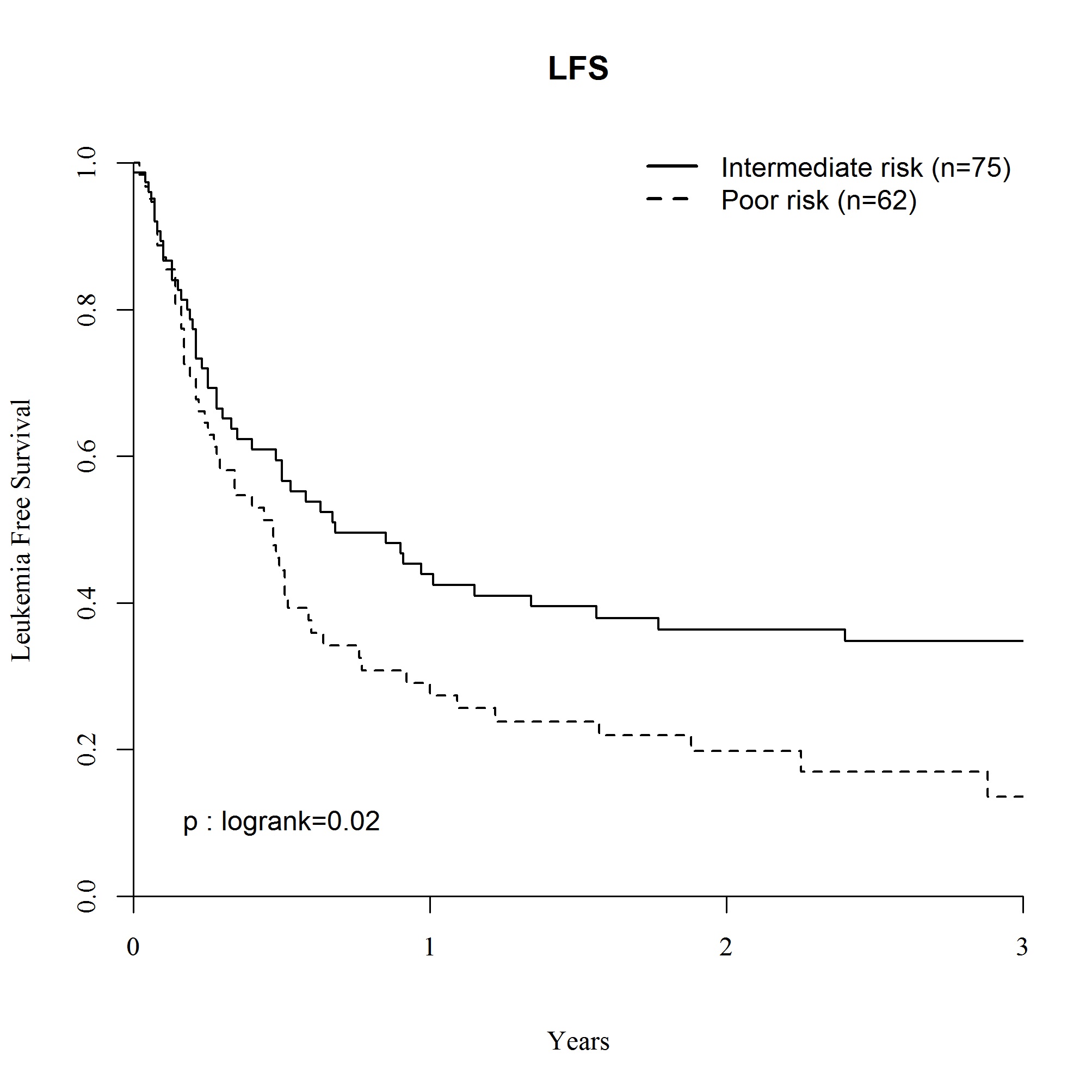
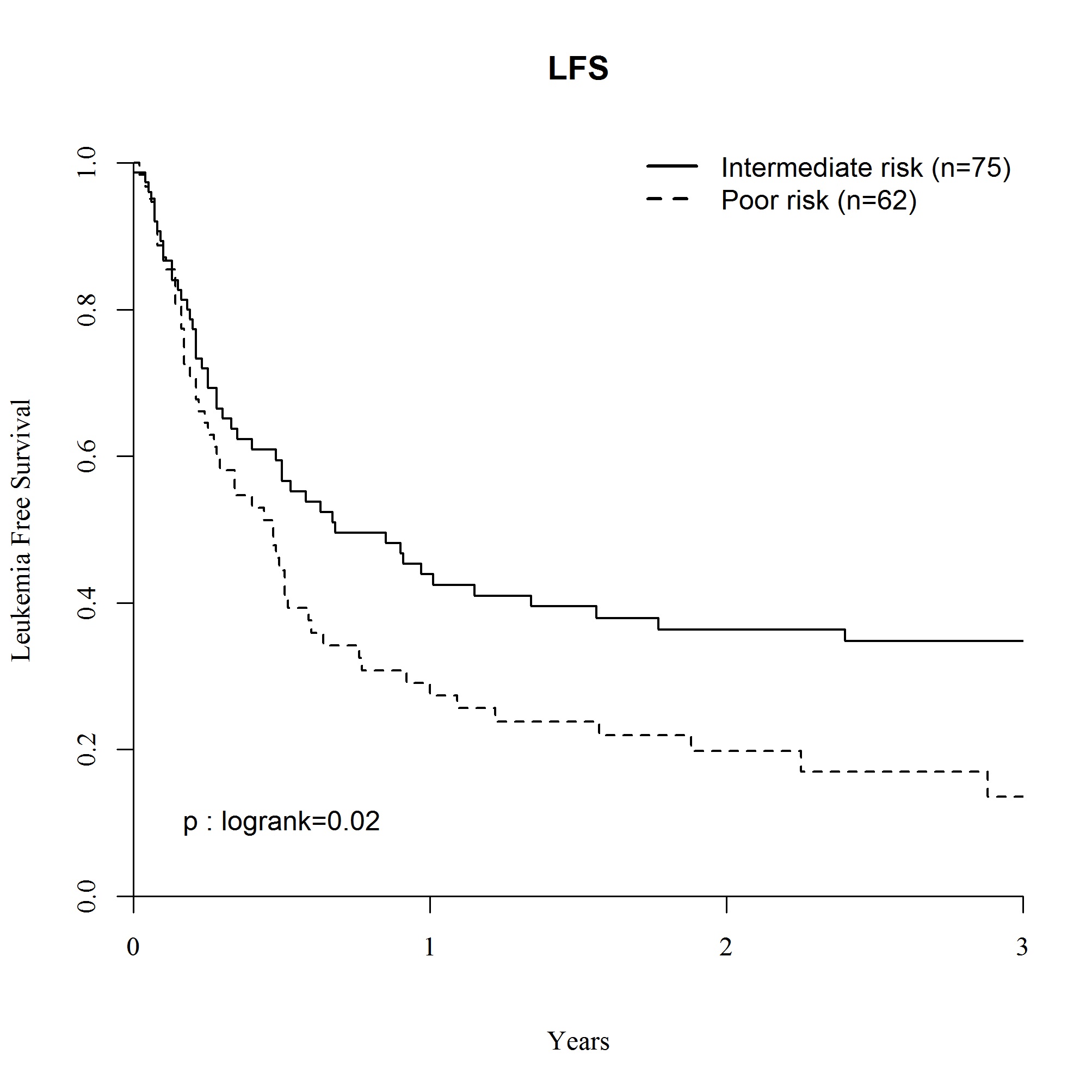
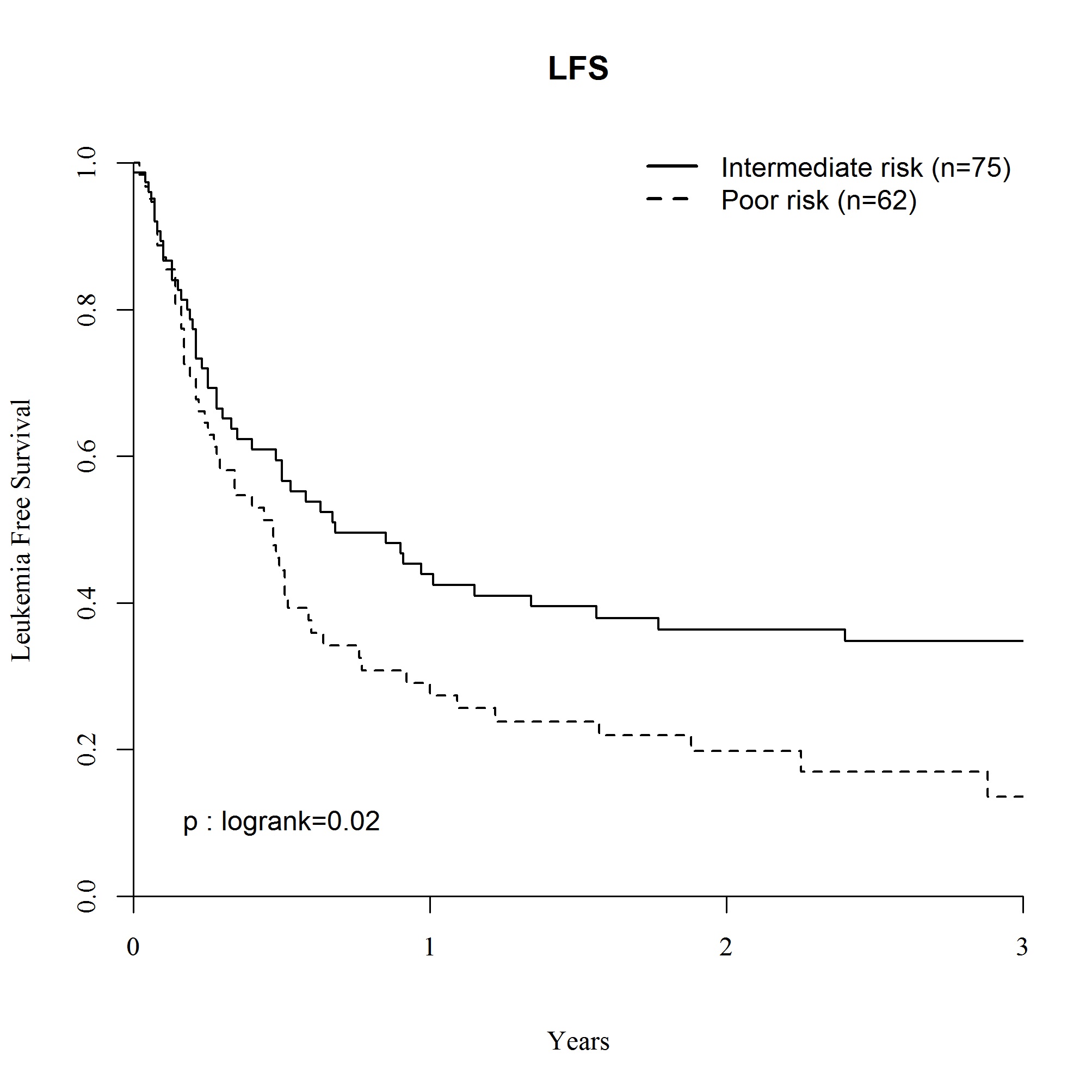
Median age was 50.5 (range, 18-74) years and 56% were males. Median time from diagnosis to allo-SCT was 111 (range, 60-178) days. 51 % received a MAC regimen, and 49% a RIC regimen. Peripheral blood stem cell (PBSC) was the main stem cell source (94.8%). The median follow-up was 18 months(range, 1.2-153). 296 patients received a matched UD (10/10) and 85 a mismatched UD (9/10). Engraftment was achieved in 95.2% of cases. 70.4% patients reached CR after allo-SCT. At 2 years, the cumulative incidences of acute GVHD≥2 and chronic GVHD (cGVHD) were 35.5% and 25.8%, respectively. At 2 years, OS and LFS rates were 34.3% and 28.3%. RI was 46.4% and NRM 25.1%. In multivariate analysis, 2 predictive factors were associated with lower OS: cytogenetics (poor vs intermediary; HR=2.00, 95%CI,1.25-3.18, p=0.004) and positive CMV status of the recipient (HR=1.52, 95%CI,1.09-2.11, P=0.01), whereas Karnofsky status at transplant ≥80% (KS) was associated with better OS (HR=0.65, 95%CI,0.43-0.98, p=0.04) (Fig1). The same factors were predictive for LFS: cytogenetics (HR=1.86, 95%CI,1.19-2.92, p=0.01) and positive CMV status of the recipient (HR=1.46, 95%CI, 1.07-1.99, p=0.02) were negative predictive factors, whereas KS was a positive one (HR=0.61, 95%CI,0.41-0.91, p=0.02). In multivariate analysis for RI, cytogenetics was the only risk factor associated with increased relapse (HR=1.92, 95%CI,1.15-3.19, p=0.001). As for NRM, patient gender (female vs male) and KS were factors associated with lower NRM (HR=0.49, 95%CI,0.29-0.84, p=0.01; HR=0.41, 95%CI,0.22-0.76, p=0.004), while CMV positive status was the only factor associated with higher NRM (HR=1.96, 95%CI=1.11-3.43, p=0.02).
Summary
Unrelated donor transplantation (10/10 or 9/10) may rescue about one third of the patients with primary refractory AML. Moreover, this study identifies cytogenetics, KS, and CMV status as major prognostic factors. Finally, these data pave the way not only for improving patients’ selection, but also for investigating more intensive additional approaches relying on sequential conditioning regimens (debulking phase followed by RIC) and/or post-transplant treatments such as 5-azacytidine, prophylactic donor lymphocytes infusions, or targeted therapy which further improve results in this devastating group of patients.
Keyword(s): Acute myeloid leukemia, Allo-SCT, Clinical outcome, Prognostic factor
Session topic: Stem cell transplantation: Clinical 1
Type: Oral Presentation
Presentation during EHA20: From 12.06.2015 12:00 to 12.06.2015 12:15
Location: Room Lehar 1 + 2
Background
Primary refractory AML is associated with a dismal prognosis. Approximately one third of patients younger than 60 years, and 50 % of older patients, with newly diagnosed AML fail to achieve complete remission (CR) with standard induction chemotherapy. Allo-SCT in the setting of active disease is an alternative but highly debatable strategy. The increased availability of UD and the use of reduced-intensity conditioning (RIC) regimens have opened the possibility for transplantation to a larger number of patients in comparison to standard myeloablative regimens (MAC)
Aims
The current study aimed to assess outcomes in a cohort of 381 primary refractory AML patients who received allo-SCT from an UD (10/10 or 9/10). Primary refractoriness was defined as failure to achieve CR within 60 days after starting induction.
Methods
Patients with primary refractory AML reported between 2000 and 2013 to the registry of the Acute Leukemia Working Party of the EBMT were included in this study. The major endpoints were to assess overall survival (OS), leukemia-free survival (LFS), relapse incidence (RI), and non relapse mortality (NRM).
Results
Median age was 50.5 (range, 18-74) years and 56% were males. Median time from diagnosis to allo-SCT was 111 (range, 60-178) days. 51 % received a MAC regimen, and 49% a RIC regimen. Peripheral blood stem cell (PBSC) was the main stem cell source (94.8%). The median follow-up was 18 months(range, 1.2-153). 296 patients received a matched UD (10/10) and 85 a mismatched UD (9/10). Engraftment was achieved in 95.2% of cases. 70.4% patients reached CR after allo-SCT. At 2 years, the cumulative incidences of acute GVHD≥2 and chronic GVHD (cGVHD) were 35.5% and 25.8%, respectively. At 2 years, OS and LFS rates were 34.3% and 28.3%. RI was 46.4% and NRM 25.1%. In multivariate analysis, 2 predictive factors were associated with lower OS: cytogenetics (poor vs intermediary; HR=2.00, 95%CI,1.25-3.18, p=0.004) and positive CMV status of the recipient (HR=1.52, 95%CI,1.09-2.11, P=0.01), whereas Karnofsky status at transplant ≥80% (KS) was associated with better OS (HR=0.65, 95%CI,0.43-0.98, p=0.04) (Fig1). The same factors were predictive for LFS: cytogenetics (HR=1.86, 95%CI,1.19-2.92, p=0.01) and positive CMV status of the recipient (HR=1.46, 95%CI, 1.07-1.99, p=0.02) were negative predictive factors, whereas KS was a positive one (HR=0.61, 95%CI,0.41-0.91, p=0.02). In multivariate analysis for RI, cytogenetics was the only risk factor associated with increased relapse (HR=1.92, 95%CI,1.15-3.19, p=0.001). As for NRM, patient gender (female vs male) and KS were factors associated with lower NRM (HR=0.49, 95%CI,0.29-0.84, p=0.01; HR=0.41, 95%CI,0.22-0.76, p=0.004), while CMV positive status was the only factor associated with higher NRM (HR=1.96, 95%CI=1.11-3.43, p=0.02).
Summary
Unrelated donor transplantation (10/10 or 9/10) may rescue about one third of the patients with primary refractory AML. Moreover, this study identifies cytogenetics, KS, and CMV status as major prognostic factors. Finally, these data pave the way not only for improving patients’ selection, but also for investigating more intensive additional approaches relying on sequential conditioning regimens (debulking phase followed by RIC) and/or post-transplant treatments such as 5-azacytidine, prophylactic donor lymphocytes infusions, or targeted therapy which further improve results in this devastating group of patients.
Keyword(s): Acute myeloid leukemia, Allo-SCT, Clinical outcome, Prognostic factor
Session topic: Stem cell transplantation: Clinical 1
Abstract: S128
Type: Oral Presentation
Presentation during EHA20: From 12.06.2015 12:00 to 12.06.2015 12:15
Location: Room Lehar 1 + 2
Background
Primary refractory AML is associated with a dismal prognosis. Approximately one third of patients younger than 60 years, and 50 % of older patients, with newly diagnosed AML fail to achieve complete remission (CR) with standard induction chemotherapy. Allo-SCT in the setting of active disease is an alternative but highly debatable strategy. The increased availability of UD and the use of reduced-intensity conditioning (RIC) regimens have opened the possibility for transplantation to a larger number of patients in comparison to standard myeloablative regimens (MAC)
Aims
The current study aimed to assess outcomes in a cohort of 381 primary refractory AML patients who received allo-SCT from an UD (10/10 or 9/10). Primary refractoriness was defined as failure to achieve CR within 60 days after starting induction.
Methods
Patients with primary refractory AML reported between 2000 and 2013 to the registry of the Acute Leukemia Working Party of the EBMT were included in this study. The major endpoints were to assess overall survival (OS), leukemia-free survival (LFS), relapse incidence (RI), and non relapse mortality (NRM).
Results
Median age was 50.5 (range, 18-74) years and 56% were males. Median time from diagnosis to allo-SCT was 111 (range, 60-178) days. 51 % received a MAC regimen, and 49% a RIC regimen. Peripheral blood stem cell (PBSC) was the main stem cell source (94.8%). The median follow-up was 18 months(range, 1.2-153). 296 patients received a matched UD (10/10) and 85 a mismatched UD (9/10). Engraftment was achieved in 95.2% of cases. 70.4% patients reached CR after allo-SCT. At 2 years, the cumulative incidences of acute GVHD≥2 and chronic GVHD (cGVHD) were 35.5% and 25.8%, respectively. At 2 years, OS and LFS rates were 34.3% and 28.3%. RI was 46.4% and NRM 25.1%. In multivariate analysis, 2 predictive factors were associated with lower OS: cytogenetics (poor vs intermediary; HR=2.00, 95%CI,1.25-3.18, p=0.004) and positive CMV status of the recipient (HR=1.52, 95%CI,1.09-2.11, P=0.01), whereas Karnofsky status at transplant ≥80% (KS) was associated with better OS (HR=0.65, 95%CI,0.43-0.98, p=0.04) (Fig1). The same factors were predictive for LFS: cytogenetics (HR=1.86, 95%CI,1.19-2.92, p=0.01) and positive CMV status of the recipient (HR=1.46, 95%CI, 1.07-1.99, p=0.02) were negative predictive factors, whereas KS was a positive one (HR=0.61, 95%CI,0.41-0.91, p=0.02). In multivariate analysis for RI, cytogenetics was the only risk factor associated with increased relapse (HR=1.92, 95%CI,1.15-3.19, p=0.001). As for NRM, patient gender (female vs male) and KS were factors associated with lower NRM (HR=0.49, 95%CI,0.29-0.84, p=0.01; HR=0.41, 95%CI,0.22-0.76, p=0.004), while CMV positive status was the only factor associated with higher NRM (HR=1.96, 95%CI=1.11-3.43, p=0.02).
Summary
Unrelated donor transplantation (10/10 or 9/10) may rescue about one third of the patients with primary refractory AML. Moreover, this study identifies cytogenetics, KS, and CMV status as major prognostic factors. Finally, these data pave the way not only for improving patients’ selection, but also for investigating more intensive additional approaches relying on sequential conditioning regimens (debulking phase followed by RIC) and/or post-transplant treatments such as 5-azacytidine, prophylactic donor lymphocytes infusions, or targeted therapy which further improve results in this devastating group of patients.
Keyword(s): Acute myeloid leukemia, Allo-SCT, Clinical outcome, Prognostic factor
Session topic: Stem cell transplantation: Clinical 1
Type: Oral Presentation
Presentation during EHA20: From 12.06.2015 12:00 to 12.06.2015 12:15
Location: Room Lehar 1 + 2
Background
Primary refractory AML is associated with a dismal prognosis. Approximately one third of patients younger than 60 years, and 50 % of older patients, with newly diagnosed AML fail to achieve complete remission (CR) with standard induction chemotherapy. Allo-SCT in the setting of active disease is an alternative but highly debatable strategy. The increased availability of UD and the use of reduced-intensity conditioning (RIC) regimens have opened the possibility for transplantation to a larger number of patients in comparison to standard myeloablative regimens (MAC)
Aims
The current study aimed to assess outcomes in a cohort of 381 primary refractory AML patients who received allo-SCT from an UD (10/10 or 9/10). Primary refractoriness was defined as failure to achieve CR within 60 days after starting induction.
Methods
Patients with primary refractory AML reported between 2000 and 2013 to the registry of the Acute Leukemia Working Party of the EBMT were included in this study. The major endpoints were to assess overall survival (OS), leukemia-free survival (LFS), relapse incidence (RI), and non relapse mortality (NRM).
Results
Median age was 50.5 (range, 18-74) years and 56% were males. Median time from diagnosis to allo-SCT was 111 (range, 60-178) days. 51 % received a MAC regimen, and 49% a RIC regimen. Peripheral blood stem cell (PBSC) was the main stem cell source (94.8%). The median follow-up was 18 months(range, 1.2-153). 296 patients received a matched UD (10/10) and 85 a mismatched UD (9/10). Engraftment was achieved in 95.2% of cases. 70.4% patients reached CR after allo-SCT. At 2 years, the cumulative incidences of acute GVHD≥2 and chronic GVHD (cGVHD) were 35.5% and 25.8%, respectively. At 2 years, OS and LFS rates were 34.3% and 28.3%. RI was 46.4% and NRM 25.1%. In multivariate analysis, 2 predictive factors were associated with lower OS: cytogenetics (poor vs intermediary; HR=2.00, 95%CI,1.25-3.18, p=0.004) and positive CMV status of the recipient (HR=1.52, 95%CI,1.09-2.11, P=0.01), whereas Karnofsky status at transplant ≥80% (KS) was associated with better OS (HR=0.65, 95%CI,0.43-0.98, p=0.04) (Fig1). The same factors were predictive for LFS: cytogenetics (HR=1.86, 95%CI,1.19-2.92, p=0.01) and positive CMV status of the recipient (HR=1.46, 95%CI, 1.07-1.99, p=0.02) were negative predictive factors, whereas KS was a positive one (HR=0.61, 95%CI,0.41-0.91, p=0.02). In multivariate analysis for RI, cytogenetics was the only risk factor associated with increased relapse (HR=1.92, 95%CI,1.15-3.19, p=0.001). As for NRM, patient gender (female vs male) and KS were factors associated with lower NRM (HR=0.49, 95%CI,0.29-0.84, p=0.01; HR=0.41, 95%CI,0.22-0.76, p=0.004), while CMV positive status was the only factor associated with higher NRM (HR=1.96, 95%CI=1.11-3.43, p=0.02).
Summary
Unrelated donor transplantation (10/10 or 9/10) may rescue about one third of the patients with primary refractory AML. Moreover, this study identifies cytogenetics, KS, and CMV status as major prognostic factors. Finally, these data pave the way not only for improving patients’ selection, but also for investigating more intensive additional approaches relying on sequential conditioning regimens (debulking phase followed by RIC) and/or post-transplant treatments such as 5-azacytidine, prophylactic donor lymphocytes infusions, or targeted therapy which further improve results in this devastating group of patients.
Keyword(s): Acute myeloid leukemia, Allo-SCT, Clinical outcome, Prognostic factor
Session topic: Stem cell transplantation: Clinical 1
{{ help_message }}
{{filter}}


